SARS-CoV-2, the virus responsible for COVID-19, has turned the world upside down. Experts have predicted that it will claim the lives of between 9-18 million worldwide. This is in addition to destroying the livelihoods, mental health and education of countless others. The pandemic will probably wreak havoc for many years to come, despite the remarkable speed of vaccine development. This is not helped by the emergence of new variants sweeping the world, which pose a serious threat to the success of vaccination and upcoming treatments.
It is difficult to predict the future pattern of SARS-CoV-2. Many scientists believe it will continue to circulate in pockets around the globe, meaning that it will become endemic in the same way as flu. In this context the number of infections remains relatively constant with occasional flare-ups that run the danger of turning into a pandemic. A lot depends on how widely the population around the world can be vaccinated and how long immunity lasts after natural infection or vaccination.
Long term, the best solution would be to develop a universal vaccine—one that would help protect against all current variants of the coronavirus and any others that arise in the future. Without it, the world runs the risk of recurrent pandemics.
Given the difficulties encountered in creating a universal flu vaccine, this may seem a tall order. But a number of scientists believe it is possible based on the rapid development of the SARS-CoV-2 vaccines.
COVID-19 is in fact the third major infectious disease outbreak to have been triggered in the last two decades by a new coronavirus jumping from animals into humans, the other two being Sars and Mers.
To get a sense of how far a pan-coronavirus vaccine has progressed we spoke to a number of key players in the field. We are both experts in this area but come at it from very different angles—Lara Marks is a historian of medicine with an interest in biotechnology and vaccines, while Ankur Mutreja has experience in tracking outbreaks and developing vaccines for infectious diseases. From our conversations, there appear to be a number of encouraging vaccine candidates on the horizon—it is even possible that one could be developed for use in humans within 12 months.
‘The holy grail’
One of the first people we spoke to was Richard Hatchett, the CEO of the Coalition for Epidemic Preparedness Innovations (Cepi). Set up in 2017, Cepi is a global partnership between public, private, philanthropic and civil society organizations that aims to compress the development of vaccines against emerging infectious diseases into 100 days—a third of the time achieved with the first COVID-19 vaccines.
Envisaging equitable access to vaccines for all countries, in January 2021, Cepi announced it would raise and invest US$3.5 billion in vaccine research and development to strengthen global preparedness to pandemics, of which US$200 million has been put aside to develop a universal coronavirus vaccine. Such a vaccine would offer protection against a broad range of coronaviruses, regardless of their variants. This would reduce the need to modify the vaccine on a regular basis.
Hatchett described these vaccines as the “holy grail.” But he argued it may take years of investment. He said: “If you want to grow a tree, the best thing to have done is to have planted it 20 years ago. And if you didn’t do that, then the next best thing is to plant it today.”
When asked about what the best vaccine would be going forward to deal with SARS-CoV-2, Hatchett replied:
We do not actually know specifically yet. This is really our first engagement with this virus, obviously, and we’ve watched it expand and unfold over time… We’re still gathering data and gaining experience on this. I think we need to have some humility about what we know currently and what we can know. We just have to be vigilant.
Why is SARS-CoV-2 mutating?
None of the scientists we interviewed were surprised to see SARS-CoV-2 mutating. All viruses mutate. They often undergo random genetic changes because the virus replication machinery is not perfect. It is a bit like a game of “telephone” where children repeat what they thought they heard, making mistakes all along the way so that the final message is very different from the original one. Whenever a virus develops one or more mutations it is considered a “variant” of the original virus.
The mutation process helps viruses to adapt and survive any onslaught from the host’s immune system, vaccination or drug treatment and natural competition. Viruses change faster when under such pressures.
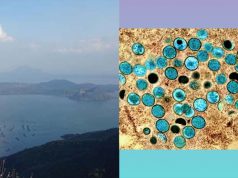
Scientists have been monitoring the genetic variations in SARS-CoV-2 since the start of the pandemic. They do this by sequencing the total RNA (genome) of the virus collected from patient samples. The genome is the complete set of genetic instructions an organism needs to function and thrive.
Scientists in China managed to sequence the first SARS-CoV-2 genome just one week after the first patient was hospitalized with unusual pneumonia in Wuhan. First drafted on January 5, 2020, the sequence revealed the virus to be a close relative of SARS-CoV-1, a human coronavirus which caused an outbreak of a severe respiratory disease SARS that first appeared in China in 2002 and then spread to many other countries. It also resembled a SARS-like coronavirus found in bats.
Comprising a single-strand of RNA, the SARS-CoV-2 genome turned out to be the longest genome of any known RNA virus. With the aid of sequencing scientists were quickly able to pinpoint the genes that carry the instructions for the spike protein, the part of the virus that helps it to invade human cells. This became an important target for the development of COVID-19 vaccine.
Initial genome sequencing data suggested that SARS-CoV-2 mutated much slower than most other RNA viruses, being half the rate of the virus responsible for flu and a quarter of that found for HIV. But its mutation rate has gathered speed over time, helped by the large reservoir of people it has infected and selection pressures.
Not all mutations are bad news. In some cases, they weaken the virus with the variant disappearing without a trace. But in other cases, they enable the virus to enter a host’s cells more easily or to escape the immune system more effectively, making it more difficult to prevent and treat.
So far, five new variants of concern have emerged with SARS-CoV-2. The first (alpha) was detected in south-east England in September 2020. Others were found shortly thereafter in South Africa (beta), Brazil (gamma), India (delta) and Peru (lambda). What is troubling about these new variants is that they are more transmissible, making them spread faster, which increases the likelihood of re-infection and a resurgence in cases. Every SARS-CoV-2 virus out there today is a variation of the original and new variants will continue to appear.
Preliminary research suggests that the first-generation of vaccines offer some protection against the new variants, helping to reduce severe disease and hospitalization. However, they will probably become less effective over time as the virus mutates further and the immunity that people have gained, either through vaccination or natural infection, wanes.
Looking for weak spots
In terms of a universal coronavirus vaccine, the ultimate question, Hatchett believes, is whether there are any weak spots that are “conserved across coronaviruses as a viral family to which you can develop immune responses that effectively protect you.”
The key issue in creating a universal vaccine is how broad a coverage the vaccine should offer. This was also pointed out to us by Andrew Ward at the Scripps Research Institute in California. As he put it:
Should it be SARS-CoV-2 and variants? Should it be SARS-1 and SARS-2? Should it be all sarbecocoviruses [a subgroup of SARS viruses of which SARS-CoV-1 and 2 are notable members] or SARS-like viruses? That’s unknown. We know that SARS viruses exist in bats and pangolins and they’ve never been as big of a problem as now. But it’s one of those things, that if it’s not really a problem do we go after it and try to proactively get vaccine programs deployed and get people either vaccinated or stockpile vaccines?
Creating a universal vaccine is itself highly challenging. For example, scientists have tried for years but not yet succeeded in developing a universal vaccine for flu. Nor have they yet managed to create one for HIV. In part, this is because the surface proteins found on these viruses frequently change their appearance. This makes it difficult for our immune system to recognize the virus.
But scientists have made enormous advances in recent years in understanding the interaction between the immune system and viruses that cause flu and HIV. They are now deploying this knowledge to build a universal vaccine for coronaviruses, which do not change as fast.
A long history of vaccine innovation
One of the reasons for optimism with a universal coronavirus vaccine is the successful development of the SARS-CoV-2 vaccine. Made in record time, the foundation for the vaccine was laid many years ago. Until the 1980s most vaccines were developed by modifying a virus or bacteria to make it no longer dangerous.
This was achieved by weakening or inactivating the pathogen so that it could be injected safely to stimulate an immune response. While highly successful for protecting against a host diseases like measles, polio, rabies and chickenpox, this approach didn’t prove effective in all diseases.
By the 1980s vaccine production stood on the cusp of change helped by the emergence of biotechnology. Where this was first successfully applied was in the development of a vaccine against hepatitis B, which is estimated to cause more deaths worldwide than TB, HIV or malaria.
The first hepatitis B vaccine was developed by Maurice Hilleman at Merck. Approved in 1981, it was the first vaccine to protect against cancer. Chronic hepatitis B is a major cause of liver cancer. In fact, it is second only to tobacco as a human carcinogen. What was novel about the hepatitis B vaccine was that instead of using the whole hepatitis B virus, which was difficult to grow in the laboratory, it used only a coat surface particle of the virus. This was a major breakthrough for vaccine technology.
Another vaccine that uses virus particles is the one against the human papillomavirus (HPV) which causes cervical cancer, a disease that globally kills 260,000 women every year. First licensed in 2005, the HPV vaccine took years to develop. It consists of tiny proteins that look like the outside of four types of real HPV produced in yeast.
Synthetic vaccines
Vaccine technology underwent a further revolution following the outbreak of the swine flu pandemic that swept the world for 19 months from January 2009. The pandemic killed between 151,700 and 575,400 people worldwide. Caused by an H1N1 influenza virus, the episode was an important reminder of the speed that pandemics can strike and the chaos they can sow. It was also a salutary lesson for companies who developed hundreds of millions of licensed vaccine doses to counter the pandemic. Although achieved within just six months, a historical record, this was not fast enough—by then the peak of infections had passed.
Part of the delay was because of the time it took to grow enough of the virus in eggs or cultured mammalian cells. Another method, using genetic engineering to produce the virus, proved much faster, but was hampered by regulatory hurdles. Determined to accelerate vaccine availability for future pandemics, from 2011, vaccine experts put in place a new strategy that took advantage of advances in genomics and the open sharing of electronic sequence data. Coupled with a new ability to synthesize genes, these tools gave scientists the power to design genome segments from a virus to prepare vaccines to train the body to recognize and target a real virus if it invaded.
Critically, the new synthetic approach moved vaccine development away from the time-consuming process of isolating and shipping viruses between different sites and then growing them at scale. All that was needed was to download the relevant sequence data from the internet and synthesize the right genes to generate relevant viral components to start vaccine development. Speed was not the only advantage the new method offered. It also reduced any potential biohazard risks involved in manufacturing the vaccine.
Attention was also paid to making the testing process more efficient. Usually the slowest part of vaccine development, such testing often takes years to complete. Tests are first conducted in animals, to assess the safety, the strength of the immune response stimulated and protective efficacy of the vaccine candidate. Once this is done it is tested in humans.
Human trials are run in three phases, each with increasing numbers of people and escalating costs. One means to reduce the time needed and cut costs was to take advantage of new biomarkers. These provided a means to measure both normal and pathological processes as well as responses to a drug. Such biomarkers made it possible to determine the toxicity and efficacy of a candidate much earlier in the clinical trial process and to run multiple trials in parallel without compromising on safety.
In 2011, a group of scientists from the companies Novartis and Synthetic Genomics, as well as the Craig Venter Institute (a non-profit research organization) proved they could develop a vaccine candidate in a matter of days.
Their approach was first successfully put to the test in March 2013 when Chinese health officials reported a novel strain of avian influenza had infected three people. Within just a week of gaining access to the virus’s genome sequence, the Novartis team, headed by Rino Rappoli, managed to create a fully synthetic RNA-based vaccine ready for pre-clinical testing, which proved safe and elicited a good immune response.
Marking the switch from what Rappouli calls “analogue vaccines” to “digital vaccines”, the 2013 work provided a template for when COVID-19 was declared a pandemic on March 11, 2020. The first dose of the COVID-19 vaccine candidate, developed by Moderna, was ready for phase I testing in humans by March 16, 2020. Many other vaccine candidates soon entered the pipeline thereafter.
New understandings
What also helped propel the first COVID-19 vaccines forward was the explosion in knowledge about the atomic structure of proteins found on the surface of viruses and antibodies that bound to them. According to Ward this was greatly helped by advances in cryo-electron microscopy which as he says “opened up the door for HIV and other pathogens.” With the technique, Ward and his colleagues discovered that coronaviruses gained entry and fused with human cells with the help of a small loop of amino acids, called S-2P, on the top of their spike proteins. This laid an important foundation for creating the COVID-19 vaccines.
Another critical development was the discovery of broadly neutralizing antibodies (bNAbs). First isolated in the early 1990s in the serum of people living with HIV-1, these antibodies only appear in some people after years of infection. Such antibodies have the advantage that they can neutralize multiple diverse strains of the virus in one stroke.
Finding the bNAbs critically opened up a new avenue for vaccine design. In particular, it offered the possibility of creating a universal vaccine against flu and also a vaccine for HIV which so far has been difficult to do because it mutates so fast. Several groups had already made progress in this field before COVID-19 struck, which they quickly turned towards coronaviruses. Their goal was to create a vaccine to stimulate the production of bNAbs targeting the receptor binding domain (RBD) located on the coronavirus’ spike protein.
One approach, outlined to us by Barton Haynes, an immunologist at Duke University, involves attaching little bits of the RBD, from multiple coronaviruses, to a protein nanoparticle for use as a vaccine candidate. Promisingly this was shown in monkeys to not only block SARS-CoV-2 and its new concerning variants but also SARS-CoV-1 and a group of bat coronaviruses which could spill over to humans in the future.
Another potential vaccine was described to us by Pamela Bjorkman, a structural immunologist at the Caltech. Her team developed it based on a virus particle platform first devised at Oxford University, in 2016. She said:
My lab really does structural biology, which means that we look at the 3D structures of the targets of the immune system, which are usually spikes that come out of the virus. So coronaviruses have the famous spikes, and so does HIV and flu.
One of the things we’ve been trying to do [for a vaccine] is to make a nanoparticle, which is a small, little thing that looks like a miniature soccer ball. And attach pieces of the spike to that using a very easy technology that was developed at Oxford University.
Their vaccine presents many different RBD fragments, from a variety of animal coronaviruses, grafted onto small proteins attached to a nanoparticle scaffolding. Tests in mice showed a single dose of the vaccine could neutralize multiple human and animal coronaviruses, including ones not included in the vaccine design.
According to our interview with Jonathan Heeney, a comparative pathologist at the University of Cambridge, his group has also developed a promising broad coverage coronavirus vaccine. Based on detailed screening of the virus’s structure they have synthesized DNA constructs to plug into conventional vaccine platforms and the latest mRNA vaccine technology.
The vector is specially designed not to trigger unintentional hyper-inflammatory responses, which can sometimes be life threatening. In animal studies, their candidate provided protection against a variety of sarbecoviruses, which cover SARS-CoV-1, SARS-CoV-2 and many bat coronaviruses.
All three outlined approaches have yet to be tested in humans. The Cambridge one is set to enter phase 1 trials in the autumn and the one at Duke University is nearing that milestone too. Both the Cambridge and Caltech candidates have the attraction that they can be produced as a heat-stable and freeze-dried powder. This will make their storage and distribution much easier than the current mRNA vaccines (Moderna and Pfizer). It will also make production much cheaper, which is vital to ensuring equitable access to the vaccine across the world and bringing the pandemic under control.
New pandemics
While scientists have the tools to develop a pan-coronavirus vaccine within a year, its creation would not be the end of the story. Growing population density, human mobility and ecological change means that the world will continue to face the threat of new pandemics.
Meeting this challenge will require a high degree of outbreak vigilance, political will and international cooperation as well as continued investment in vaccine development well beyond the end of the COVID-19 pandemic. As the WHO put it in September 2020, “a global pandemic requires a world effort to end it – none of us will be safe until everyone is safe.”
Access to vaccines is also only one arm of what is needed to combat pandemics. What SARS-CoV-2 has also taught us is the importance of rapid frontline genomic sequencing on the ground to swiftly detect newly emerging threats. As Hatchett argues, the key to radically reducing epidemic and pandemic risk to the world is through “earlier detection, earlier sequencing, and earlier more tailored public health responses.”
, Visiting Research Fellow, History of Biomedical Sciences, University of Cambridge.
, Group Leader, Global Health (Infectious Diseases), University of Cambridge.
This article is republished from The Conversation under a Creative Commons license. Read the original article.