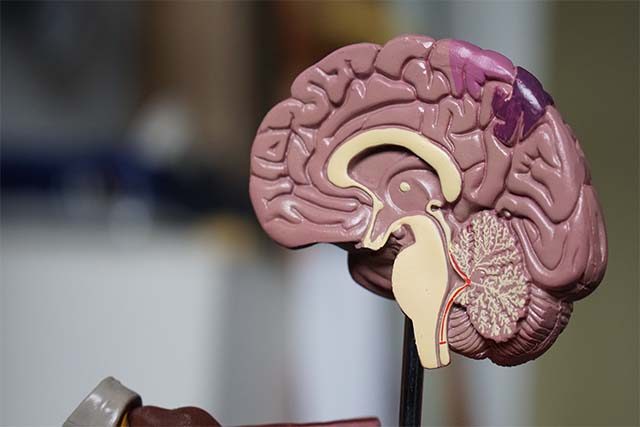
Most of what we know about how COVID can affect the brain has come from studies of severe infection. In people with severe COVID, inflammatory cells from outside the brain can enter brain tissue and spread inflammation. There may be changes to blood vessels. Brain cells can even have changes similar to those seen in people with Alzheimer’s disease.
For the first time, a new study has investigated the effects of mild COVID (that is, infection that doesn’t lead to a hospital admission) on the brain. The findings may further explain some of the brain changes contributing to long COVID.
Brain scans and tests show changes
Many people who have had COVID report feelings of “brain fog”, fatigue and problems with concentration and memory long after their initial symptoms resolve. These problems, collectively referred to as “long COVID”, may last for months even after mild infection.
Long COVID is very common, and may affect more than half of the people who catch COVID, even if they have a mild case.
Scientists collected data as part of the massive UK Biobank database. They looked at brain magnetic resonance imaging (MRI) scans and tests of brain function in 785 volunteers who were assessed before the pandemic. They then compared this to the same data collected three years later, when about half of those participants had mild COVID infection, and the other half had not caught COVID. This allowed the scientists to determine the specific effects of mild COVID infection on brain structure and function.
The group who had mild COVID an average of five months beforehand had thinning of brain tissue in several brain regions, ranging from 0.2% to around 2% compared to their pre-COVID scan. This is equivalent to between one and six years of normal brain ageing. Affected brain regions included the parahippocampal gyrus (an area related to memory) and the orbitofrontal cortex, which is located at the front of the brain and is important for smell and taste.
The post-COVID group also showed a reduction in overall brain size between their MRI scans that wasn’t seen in the non-COVID group, and had altered connections between different brain regions in the olfactory cortex, an area related to smell.
They performed worse in a test for attention and mental flexibility, a finding that was associated with volume reductions within a part of the cerebellum related to smell and social relationships.
Comparing to other illnesses
To show these changes were specific to COVID and not just related to having a respiratory illness, the scientists also looked at a group of people who had pneumonia. They did not see the same changes, confirming they are related to COVID.
Decreases in brain volume are common to many brain diseases and disorders associated with degeneration, and have been found in people with mild cognitive impairment, Alzheimer’s disease, depression and traumatic brain injury, among others.
Problems with memory and attention are also frequent for people with these diseases and disorders, indicating mild COVID infection may accelerate brain degeneration. These changes could explain the reported symptoms of long COVID, such as brain fog.
The study did not look at the mechanisms of mild COVID in the brain. However, the authors suggest this could be due to inflammation, degeneration which spreads through the brain pathways associated with smell, or sensory deprivation due to loss of smell.
The same for everyone?
So does this study prove all people who have had mild COVID infections will have these same brain changes and long-term brain degeneration? Not necessarily.
There are several important things we still do not know. This includes whether these brain changes will get worse over time, or whether they will go back to normal or previous levels of function. More research over a long time would help us understand the trajectory of brain changes.
This study also only included people aged 51–81, so we do not know whether these findings are relevant for younger people or children.
The brain changes found in this study were more pronounced in the older participants, so it could be that older people are more susceptible. Another study is needed to determine whether the same brain alterations would occur in younger people, or whether these findings are common only to older people.
There were some differences between the groups before COVID, with smaller volumes of areas deep within the brain. However, these were in different brain areas to those affected after COVID.
The scientists also found slightly reduced scores for brain functions of thinking and remembering in the group that went on to have COVID. This study did not specifically exclude people with degenerative brain conditions such as Alzheimer’s or Parkinson’s diseases, but the scientists do not think these would explain the changes they found.
Effects of different variants and vaccination unknown
Because of the nature of the study, information about the strain of COVID people were infected with was not available. So we can’t assume the findings would be the same for people with the now more prevalent Omicron strain.
We also can’t determine the effect vaccination may have in lessening brain changes. Given the timing of the study, it is likely most of the people in the post-COVID group were infected in 2020, so may not have been vaccinated.
This study provides the first important information about brain changes in people with mild COVID infection. Until we have all the information, we should be alert but not alarmed at emerging findings.![]()
Sarah Hellewell, Research Fellow, Faculty of Health Sciences, Curtin University, and The Perron Institute for Neurological and Translational Science, Curtin University. This article is republished from The Conversation under a Creative Commons license. Read the original article.