Concerned over the health of close to some 500,000 schoolchildren administered with the vaccine Dengvaxia, Senator Richard J. Gordon has expressed alarm over reports that the manufacturer Sanofi has acknowledged its dengue vaccine poses risks to certain recipients.
In what many described as a major Aha! Moment, Sanofi disclosed Thursday that, “for individuals who have not been previously infected by dengue virus, vaccination should not be recommended.”
The situation poses a big and deep quandary, especially for those responsible in the formulation and execution of this mass dengue vaccination program intended to cover one million children nine years old and up.
Click and watch a related video report from News5 below:
Early warning
Critics have noted the apparent haste that accompanied the Dengvaxia program’s rollout. Senator Gordon, chairman of the Senate Committee on Accountability of Officers and Investigations, or Blue Ribbon, said an official of the World Health Organization (WHO) had earlier warned that, at the time it was procured by the administration of then President Benigno Aquino III, the vaccine had not received pre-qualification approval.
This means the vaccine was not yet ready for distribution, explained Senator Gordon. “Now we have the evidence on that.”
Haphazard
For his part, Senator Joel Villanueva called for accountability from Sanofi as well as Department of Health officials responsible “for haphazardly allowing the vaccine to be administered without extensive due diligence on the effects and without waiting for the results of comprehensive clinical trial.”
The senator also expressed his disappointment that Sanofi had only recently revealed the result of their clinical study, after the DOH had already spent more than PhP3 billion for the program.
Senator Gordon elaborated: “Before we conducted an investigation on the anomalous procurement of this vaccine, we talked to several health experts and they told us that they had already warned government long before about the possible adverse effect of the new drug on individuals with no prior history of dengue. With this admission by Sanofi, they have been proven right.”
Sanofi acknowledgment
Sanofi acknowledged in the recent disclosure that the drug may be harmful when administered to individuals not previously infected with dengue, citing a new analysis of long-term clinical trial data that indicated that “for those not previously infected by dengue virus, more cases of severe disease could occur following vaccination upon a subsequent dengue infection.”
In effect, what Sanofi is now saying is its dengue vaccine mostly helps people who’d been previously infected by the virus.
Sanofi urged regulators to update the vaccine’s label so doctors can be guided in screening out patients who have never suffered dengue.
3 doses six months apart
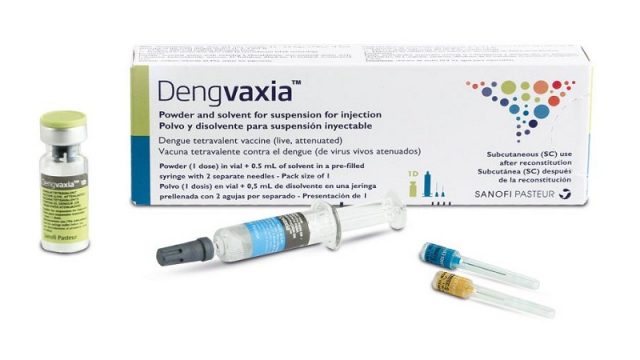
Known in the technical nomenclature as CYD-TDV, Dengvaxia is what’s called a “tetravalent, live attenuated, chimeric dengue vaccine in a yellow fever 17D backbone developed by Sanofi Pasteur.” The schedule that has been evaluated in Phase III clinical trials includes 3 doses of vaccine (at 0, 6 and 12 months).
See also:
DOH to spend P3,000 per child on dengue vaccine
Total bill: PhP3.5B
In January 2016, then Health Secretary Dr. Janette Garin told the Philippine Star that DOH was spending a total of P3.5 billion for the vaccination program for public school students in areas with high incidence of the potentially fatal disease. The initial beneficiaries of the free dengue vaccine were nine-year-old children enrolled in government schools at the National Capital Region, Central Luzon, and Calabarzon.
Garin said DOH bought the Food and Drug Administration-licensed Dengvaxia, at PhP1,000 per dose. This amount included syringes, vaccine carriers, surveillance and monitoring, and implementation costs.
Three doses were procured for one million children, each successive dose to be given every six months. The school-based dengue immunization was launched in April last year.
See:
DOH to review dengue immunization program after all doses of Dengvaxia delivered
A Philippine News Agency dispatch on that same day reported that Rep. Estrellita Suansing (1st District, Nueva Ecija) called for an inquiry, in aid of legislation, into the DOH’s school-based immunization program to scrutinize, among others, research studies on the dengue vaccine’s efficacy and safety, and determine if government standards of accountability and transparency have been followed.
WHO? No, not WHO
When critics aired misgivings about the lack of a recommendation from the World Health Organization’s Strategic Advisory Group of Experts (SAGE) at the time, DOH Secretary Garin and, later, her successor Dr. Paulyn Jean B. Rosell-Ubial were to argue that there was no legal requirement to get a certification from the WHO.
Ubial elaborated that a WHO certification is required only for United Nations (UN) procurement agencies, such as UNICEF, UNDP, and the United Nations Population Fund.
While it does not fall under the purview of the WHO to approve vaccines, national regulatory authorities who have the power to license vaccines are expected to follow their own rigorous evaluations and approval processes on the basis of the quality, safety, and efficacy of the product.
Only for high endemicity
The World Health Organization’s SAGE reviewed the evidence, and recommended that countries consider introduction of the vaccine “only in settings with high endemicity”, or high incidence of dengue.
In a report on the study The Dengue Vaccine Dilemma: Balancing the Individual and Population Risks and Benefits it was noted that “CYD-TDV [Dengvaxia] vaccination immunologically primes seronegative recipients [those who have had no prior exposure], causing their first natural dengue infection to have higher severity … vaccination in low-transmission settings with a high population of seronegatives will increase the number of hospitalized dengue cases.”
The WHO recommendations have effectively split the dengue community into those that support and challenge them. Granted, wide deployment of Dengvaxia could result in considerable public health benefit, but what, then, of the seronegative individuals who were vaccinated and potentially become at increased risk for severe disease?
Dilemma of the 9-year olds
This is the dilemma now facing the possibly hundreds of thousands of our nine-year old public school pupils who received Dengvaxia but had never previously been sick of dengue.
Have they been placed at unnecessary risk by a well-meaning but “haphazardly” executed public health policy?
An article in the independent non-profit Break Dengue, Working towards a dengue-free Philippines: a look at the country’s vaccination program, is an eye-opener. Janette Garin, the former secretary of the Health Department and the person responsible for kick starting the school-based immunization program, told the author Krizette Chu: “We started the program, during my time as Secretary of Health, because we see what a big difference the vaccine would have made if everybody had access to it.
“It’s about making something available, easily accessible. Vaccines are mostly a prerogative of the rich, and the only time the government gave the public a vaccine program was if there was extra money … If the government could afford it — and we could — why wait?
“The dengue vaccine could reduce the epidemic, and also help the Filipinos as it will relieve them of spending on hospitalization and buying the vaccine themselves.”
Dr. Lyndon Lee Suy, at the time Director of Disease Prevention and Control Bureau at the DOH, articulated some of the serious challenges: “The timing of the introduction of the dengue vaccine — it was nearly vacation time when the government started the program; the looming election, which was due to happen in a month, and which meant a change in governance and health priorities and policies; and the most pressing issue of all — the lack of the World Health Organization’s SAGE recommendation, which, while not necessary in introducing the vaccine, was used by opponents to question the introduction of Dengvaxia, leading to political vaccine resistance. (WHO has since endorsed it for use in the Philippines.)”
But wait, there’s more: 158,000 kids in Cebu
In the not too distant past, just nearly one month back, more than 158,000 children aged nine to 14 in Cebu province were administered the first dose of the vaccine offered under the community-based dengue immunization program, according to the record from the Department of Health (DOH) Region 7 office.
DOH-Region 7 medical officer Dr. Shelbay Blanco told The Freeman news service that, during the initial screening, some children were found ineligible for vaccination due to such reasons as the child may be allergic to vaccines or had an allergic reaction to a prior dose, among others.
But, like the hundreds of thousand others who had already received the vaccine, they were not screened for whether or not they had contracted dengue before.
The latest word, so far
In the most recent version of a posted FAQ, this is what WHO has to say:
What are the preliminary results from the recent analysis of vaccine safety in persons seronegative to dengue prior to vaccination?
“While vaccinated trial participants overall had a reduced risk of virologically-confirmed severe dengue and hospitalizations due to dengue, the subset of trial participants who had not been exposed to dengue virus infection prior to vaccination had a higher risk of more severe dengue and hospitalizations due to dengue compared to unvaccinated participants, regardless of age. This increased risk was observed after an initial protective period and persisted over the observation period of up to 66 months post primary vaccination.”
Scratching her head, one mother at a barangay health kiosk quipped that there’s no turning back the clock now, “but how do you do right by the hundreds of thousand children who are dengue virgins but could suffer from a dengue attack made unnecessarily cruel by the vaccine?”